As much of America enters its seventh month of quarantine measures, more than 200,000 people have died from the coronavirus, and the mental and financial health of the country is wearing thin. Hopes of returning to normalcy are now pinned on one thing: finding a vaccine.
Developing, testing and distributing a vaccine is normally a years-long process, but the public need for a COVID-19 vaccine has triggered an unprecedented, accelerated response — so much so that the Trump administration dubbed its team tasked with delivering 300 million doses of a successful vaccine “Operation Warp Speed.”
Efforts to rapidly test, manufacture and distribute a vaccine, however, have left some people skeptical of its safety. Public health officials, including the director of the Centers for Disease Control and Prevention, have repeatedly offered assurances that the COVID-19 vaccine will be scrutinized to the same extent as any other vaccine. According to William Moss, executive director of Johns Hopkins’ International Vaccine Access Center, this is the most “important message” for people to understand.
Accelerating the timeline “doesn’t necessarily mean we are cutting corners on efficacy and safety,” he said, adding that “there are ways to speed things up.”
According to Moss, the key reason acceleration is possible is because the U.S. government and major pharmaceutical companies are working together to build the manufacturing capacity necessary for widespread production before the vaccine is even approved. The move is unprecedented because it is a huge financial gamble.
“Rather than eliminating steps from traditional development timelines, steps will proceed simultaneously,” reads an Operation Warp Speed fact sheet created by the Department of Health and Human Services. In order to “proceed simultaneously,” the team has authorized manufacturing of the vaccine to begin while the testing process is still underway. According to the HHS, the head start on manufacturing only increases the financial risk, “not the product risk.”
Pharmaceutical giant Pfizer, which is among the companies developing a vaccine, has already begun its manufacturing process, CEO Albert Bourla recently told CBS News’ “Face the Nation.” According to Bourla, studies from Pfizer indicate there’s “a good chance” of knowing if the company’s vaccine works “by the end of October.”
“We have already manufactured hundreds of thousands of doses,” he said, so the company “will be ready” once it gets approved by the FDA.
Pfizer rejected federal dollars for its vaccine candidate, opting instead to fully absorb the financial hit if its vaccine fails. Bourla said the decision was an attempt to shield the company from politics.
But among the most pressing issues of the presidential election is President Trump’s handling of the pandemic, and Mr. Trump has pushed hard for rapid vaccine development, disputing its timeline with the government’s top scientists.
In a White House press conference with reporters last week, Mr. Trump contradicted CDC Director Robert Redfield’s estimate of the timing for a vaccine, insisting Redfield “made a mistake” when he told Congress that the shots wouldn’t be widely available to the general public until the second or third quarter of next year.
“I believe he was confused,” Mr. Trump said of Redfield’s testimony, although Redfield appeared confident in his assessment when he testified about it before Congress earlier in the day.
“I think there will be vaccine that will initially be available some time between November and December, but very limited supply, and it will have to be prioritized,” Redfield told lawmakers. “If you’re asking me when is it going to be generally available to the American public so we can begin to take advantage of vaccine to get back to our regular life, I think we’re probably looking at late second quarter, third quarter 2021.”
Following the president’s criticism, the CDC issued a statement essentially standing by Redfield’s comments, though suggesting he might have misheard the question. It read: “In today’s hearing, Dr. Redfield was answering a question he thought was in regard to the time period in which all Americans would have completed their Covid vaccination, and his estimate was by the second or third quarter of 2021. He was not referring to the time period when Covid-19 vaccine doses would be made available to all Americans.”
A spokesperson for the CDC later retracted the statement, saying Redfield did not sign off on the reframing of his congressional testimony.
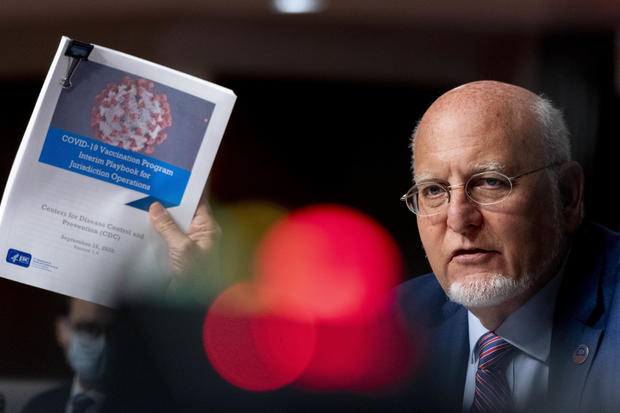
Andrew Harnik / Getty Images
As it stands, there are now eight companies with vaccines in Phase 3 clinical trials, the final phase of vaccine development which involves large-scale tests on at least 30,000 people. Phase 3 trials are the first time a company documents efficacy — how well the vaccine does at protecting participants from catching the virus, according to Moss. Phases 1 and 2 look for immunogenicity — the capacity of a vaccine to elicit an immune response in the body. All three phases assess safety.
Pfizer and Moderna, another prominent U.S. company, are both in Phase 3 trials, as is the British-Swedish company AstraZeneca, which is working with Oxford University on its large-scale human trials. According to Moss, these three companies are currently the furthest along in enrolling participants.
Johnson & Johnson’s Janssen Pharmaceuticals became the latest to start a Phase 3 trial of its vaccine candidate in September, with a study involving up to 60,000 volunteers in the U.S. and seven other countries. Unlike the other vaccines being tested, this one would only require a single dose instead of two shots.
Signing a safety pledge
All of the drugmakers involved signed a pledge earlier this month saying they would not release a vaccine until it has been proven safe and effective.
Other countries, like Russia and China, have already begun distributing their own vaccines without having completed the same types of clinical trials. Russian President Vladimir Putin claimed last month that his country was the first to develop a safe and effective vaccine. His announcement was immediately met with skepticism from both Dr. Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases, and U.S. Health Secretary Alex Azar.
Fauci said that if the U.S. “wanted to take the chance of hurting a lot of people or giving them something that doesn’t work,” it could also release a vaccine that quickly — but would not do so. “We could start doing this, you know, next week if we wanted to. But that’s not the way it works,” he said.
Moderna president Stephen Hoge told CBS News’ Norah O’Donnell last week that his company feels the pressure to produce a vaccine, whether or not it’s coming from the White House. “We haven’t been feeling direct political pressure, but definitely feel the social pressure of this moment,” Hoge said. “The goal of developing a vaccine is not to get a vaccine approved, it’s to stop the pandemic.”
Moderna took a step for transparency last week by releasing a 135-page-long fully unredacted protocol of its ongoing clinical trial, detailing how the company will determine if its vaccine is safe and effective.
It describes the trial as “randomized, stratified, observer-blind, and placebo-controlled.” Participants have been randomly assigned to receive injections of either the vaccine or a placebo, before and after which they must submit to a nasopharyngeal swab for coronavirus testing and provide a blood sample.
So far, over 25,000 of the 30,000 participants needed have enrolled in Moderna’s study, according to Hoge. Once they’ve been given either the vaccine or a placebo, they are free to engage in their normal lives — while abiding by pandemic precautions, such as mask wearing and social distancing — as the company tracks whether or not they go on to contract the coronavirus, and how sick they get if they do.
According to Moss, when looking for vaccine trial participants, companies try to find people who are representative of the “target populations” for the initial vaccine — i.e., high risk individuals. “There are efforts to include people at high risk of infection and disease as these people will be prioritized to be vaccinated,” Moss explained.
“In designing the trials, investigators try to set up the studies in communities where virus transmission is occurring,” he said. “Someone who practices strict physical distancing can participate in a vaccine trial but is less likely to become infected and develop disease so are less informative in a trial.”
Asked last week when Moderna will know if its vaccine is working, Hoge said “it’s very hard to know for sure,” explaining that the company is currently playing a waiting game.
“Now we’re going to depend upon those people unfortunately getting sick,” he said. “Our best estimates of the earliest it could happen would be the early part or the late part of the fall, November/December time horizon. But it could happen much later, or sooner, depending upon the rate of transmission in the country.”
How effective would it be?
To be approved by the Food and Drug Administration, a COVID-19 vaccine must prevent or decrease the severity of the disease in at least 50% of vaccinated people. Dr. Kathryn Edwards, who is on Pfizer’s vaccine safety committee, told “CBS This Morning” last month that even if that threshold is met, COVID-19 won’t be wiped out.
“If the vaccine’s 50% effective, it’s not going to reduce all the disease,” Edwards said. “There’s social distancing, the masks, these things may need to continue and people will continue to need to have some thought about what their activities have and the implications that they have for the rest of the community.”
Moss said the goal of 50% effectiveness means “vaccine recipients are half as likely to develop disease than the comparison group.”
“There is no specified time frame to determine efficacy. What drives the time frame is how frequently disease occurs in those who receive the study vaccine compared to those who receive the placebo vaccine,” he explained. “During a pandemic this can happen faster than in a non-pandemic situation.”
If we were not in the midst of a global pandemic, Phase 3 vaccine trials would likely take at least two to three years, and manufacturing would only begin after a formal review of the data was complete, Moss said.
Throughout the course of a typical clinical trial, two separate entities, one blinded and the other “unblinded,” examine the incoming data for efficacy and safety, Moss explained. An “independent Data and Safety Monitoring Board” is unblinded, meaning they know which participants received the vaccine and which received the placebo. This board periodically examines the data, and, because they’re unblinded, are able to assess whether the vaccine is causing harm, in which case they can quickly stop the study. On the other hand, if the vaccine is clearly beneficial, they may recommend an end to the placebo, he said. The second entity, “study investigators,” are blind as to which participants received the vaccine or placebo until the very end.
Trial participants in Pfizer’s study are required to self-monitor and log any symptoms they experience on an app, recording their temperature and any reactions every day for a week after each injection. They will be asked to continue logging any symptoms on a weekly basis for two years. Moderna participants will also be required to keep track of symptoms for two years.
Time is essential in vaccine trials. According to Moss, most adverse effects from a vaccine occur within the first month or two, but issues can also crop up long after they are administered, which is why companies keep following participants for at least two years.
AstraZeneca temporarily halted its Phase 3 trial earlier this month after one participant suffered what may have been a serious adverse reaction. The trial was later restarted after scientists scrutinized the data to determine whether the condition was related to the drug.
Moss acknowledged that having several companies simultaneously working towards the same goal implies competition; however, he said, crossing the finish line of this unique race will only be possible if everyone is running. That’s because the U.S. will need multiple manufacturers to meet demand, and one vaccine could turn out to be best suited for a distinct group, like the elderly.
“I anticipate that we will have multiple vaccines on the market, both in the United States and globally,” he said.
If any of the vaccines currently in trials receives what is called an Emergency Use Authorization, or EUA, from the FDA, the company could release the vaccine prior to the completion of Phase 3 trials. An EUA does not require as much proof as the more exhaustive FDA approval process, but can expedite treatments deemed beneficial in an emergency.
Since Phase 3 trials typically enroll 30,000 people, it’s possible that rare adverse effects from a vaccine — which occur in about one in a million people — could go undetected until it is released into the general population. And distributing a vaccine before the Phase 3 trial is complete would mean the vaccine would be available, to some extent, before long-term effects could possibly be known.
“That’s the trade off with any EUA, there just will not be long-term data,” Moss said.
Despite not having that time-tested reassurance, Moss said he expects there will be enough data on efficacy by the end of this year to warrant an authorization. He added that EUAs are only granted when there is evidence of potential benefit, and no alternatives.
“As a society we’ll have to make a trade-off decision,” he said. “What are the benefits of getting early approval, and the uncertainties around potential, rare, delayed side effects.” Ultimately, he said, the FDA will be left to determine when the “benefit outweighs the risk.”