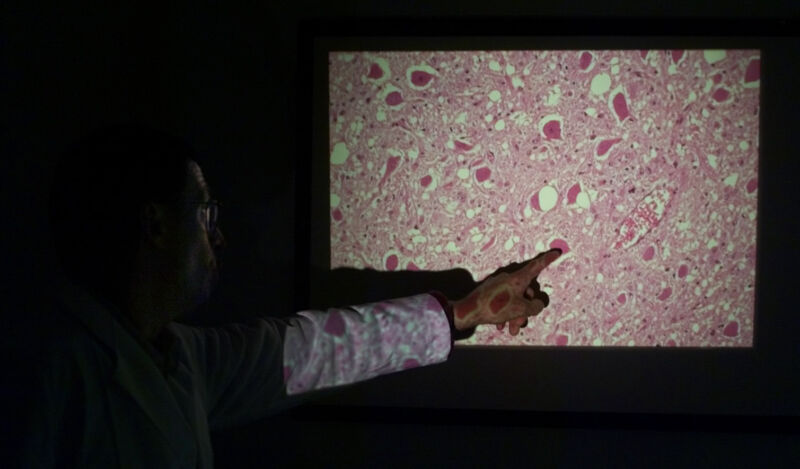
/ A pathologist examines brain tissue of a diseased deer. The white circular shapes are the sponge-like holes found with prion-related diseases called transmissable spongiform encephalopathies (TSEs).
Five public research institutions in France announced a three-month moratorium on prion research this week, following a newly identified case of prion disease in a retired lab worker.
If the case is found to be linked to a laboratory exposure, it would be the second such case identified in France. In 2019, another lab worker in the country died of a prion disease at the age of 33. Her death came around nine years after she accidentally jabbed herself in the thumb with forceps used to handle frozen slices of humanized mouse brains infected with prions.
Prions and disease
Prions are misfolded, misshapen forms of normal proteins, called prion proteins, which are commonly found in human and other animal cells. What prion proteins do normally is still unclear, but they’re readily found in the human brain. When a misfolded prion enters the mix, it can corrupt the normal prion proteins around them, prompting them to misfold as well, clump together, and corrupt others. As the corruption ripples through the brain, it leads to brain tissue damage, eventually causing little holes to form. This gives the brain a sponge-like appearance and is the reason prion diseases are also called transmissible spongiform encephalopathies (TSEs).
Outward symptoms of TSEs can include rapidly developing dementia, painful nerve damage, confusion, psychiatric symptoms, difficulty moving and/or speaking, and hallucinations. There are no vaccines or treatments for TSEs. They often progress rapidly and are always fatal.
The most common type of TSE in humans is Creutzfeldt-Jakob disease (CJD), which has two forms: “classic” and “variant.” The classic form strikes about one person in a million in the US and other countries, and patients typically die within a year of the onset of symptoms. In roughly 85 percent of classic CJD patients, the disease is found to be sporadic. That is, there’s no clear explanation of what sparked the protein misfolding. In about 5 percent to 15 percent of cases, the disease is determined to be hereditary, linked to a family history of CJD or a mutation in a prion protein that’s linked to misfolding. In extremely rare cases, classic CJD can also be acquired, usually through prion-contaminated medical procedures, such as a cornea transplant.
Variant CJD, on the other hand, is an infectious type, and it’s often associated with bovine spongiform encephalopathy (BSE), aka “mad cow” disease. People can contract variant CJD by eating prion-contaminated meat, which appeared to be the case in a large outbreak of BSE among cattle and variant CJD among people in the United Kingdom during the 1980s and 1990s. It also seems possible to develop variant CJD through prion-infected wounds, and prions may even be able to spread in aerosols—at least researchers have shown that it’s possible in mice. Once an exposure occurs, variant CJD tends to incubate for around 10 years. That is, symptoms show up around a decade after the prion exposure.
Émilie Jaumain
Importantly, the classic and variant forms of CJD have distinct clinical and pathological features. For one thing, classic CJD tends to afflict older adults (median age of death is 68), while the variant form tends to strike earlier (median age at death is 28). Classic CJD may start with memory problems and confusion, while variant CJD may start with psychiatric symptoms and painful nerve damage.
Variant CJD was the clear cause of the 2019 prion disease in the young lab worker, named Émilie Jaumain. In May of 2010, a 24-year-old Jaumain was working in a prion lab in Frances’ National Research Institute for Agriculture, Food and Environment (INRAE) when she tragically stabbed her thumb, piercing through a double-layer of latex gloves and drawing blood. “Émilie started worrying about the accident as soon as it had happened, and mentioned it to every doctor she saw,” her widower, Armel Houel, told Science Magazine.
According to a case report of her disease and death published in the New England Journal of Medicine last year, Jaumain first developed symptoms in November 2017, about 7.5 years after the accident. The symptoms started as burning pain in her right shoulder and neck, which worsened and spread to the right half of her body over the next six months. In January 2019, she became depressed and anxious and had memory impairment and visual hallucinations. The muscles on the right side of her body stiffened. According to an association set up in Jaumain’s name to promote lab safety, she was diagnosed with variant CJD in April 2019, and, before her death in June, lost the ability to move and speak. Postmortem analysis included in the NEJM case report confirmed the diagnosis of variant CJD.
Researchers cannot entirely rule out the possibility that Jaumain developed variant CJD after eating contaminated meat. However, the authors of the NEJM report noted that the last similar case of variant CJD in France died in 2014. The authors concluded that the risk of developing variant CJD in France in 2019 was “negligible or nonexistent.”
Lab safety
The authors also note that the occupational cases of variant CJD are not unheard of. “The last known Italian patient with variant CJD, who died in 2016, had had occupational contact with BSE-infected brain tissues, although subsequent investigation did not disclose a laboratory accident,” the authors wrote.
So far, little is known about the new case in France that prompted the moratorium this week. In a joint statement announcing the moratorium, the research institutions said that it was not yet known if the retired researcher, who also worked at the INRAE, had variant or classic CJD.
“The suspension period put in place as of this day will make it possible to study the possibility of a link between the observed case and the person’s former professional activity and to adapt, if necessary, the preventive measures in force in the research laboratories,” the joint statement, released Tuesday, reads.
According to reporting by Science magazine, Jaumain’s family has filed both criminal charges and an administrative lawsuit against the INRAE. The family’s lawyer told the magazine that she had not been properly trained to safely handle dangerous prions, did not wear metal mesh or surgical gloves, and did not immediately soak the thumb in bleach, which the lawyer said should have been done.
Prion decontamination is notoriously difficult. The World Health Organization recommends decontaminating waste materials by soaking them in a high concentration of bleach for an hour, then putting them in an autoclave (a steam- and pressure-based sterilization machine) at or above 121° Celsius (~250° Fahrenheit) for an hour. That said, for skin punctures, the WHO suggests people should “gently encourage bleeding” and wash the wound with soap and water.
French investigators identified 17 other lab accidents involving prions in the past decade in the country, five of which involved cuts or stabs, Science noted. Some labs have said they had improved safety in light of Jaumain’s death, such as by using plastic tools that are less sharp than metal ones and using cut-resistant gloves.