Summary: A specific group of fungi in the intestines may protect against intestinal injury and influence social behaviors.
Source: Weill Cornell Medicine
A specific group of fungi residing in the intestines can protect against intestinal injury and influence social behavior, according to new preclinical research by scientists at Weill Cornell Medicine.
The findings extend a growing body of work identifying a “gut-immunity-brain axis,” a signaling system that may have a wide range of effects on physiology in both health and disease, influenced not only by the body’s own cells but also the resident microbes.
The study, published Feb. 16 in Cell, reveals a novel set of molecular signals connecting fungi in the gut to their host’s cells throughout the body, including immune cells and neurons.
“We have made a direct link between a major immune pathway induced by fungi in the lining of the intestine and signals in the nervous system that impact animal behavior,” said senior author Dr. Iliyan Iliev, associate professor of immunology in medicine in the Division of Gastroenterology and Hepatology and a member of the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine.
Drs. Dilek Colak, Melanie Johncilla and Megan Allen from Weill Cornell Medicine and Dr. Rhonda K. Yantiss from Weill Cornell Medicine and NewYork-Presbyterian also contributed to this study.
The lining of the intestine must balance conflicting needs, absorbing water and nutrients from food while acting as a barrier to prevent the vast population of microbes in the gut from invading the bloodstream.
Examining this system in a mouse model, the scientists mapped the locations of different fungi within the intestine and found that a unique consortium of fungi tends to accumulate at specific sites near the gut epithelium, or lining, suggesting that these species have colonized the gut and interact closely with the nearby epithelial cells.
Mice carrying some of these fungi enjoyed better protection against events that can disrupt the intestinal barrier, such as intestinal injury and bacterial infection. “There was fortification of those barrier functions when we added that specific fungal community to mice,” Dr. Iliev said.
Improving intestinal barrier integrity wasn’t the only effect of the fungi. In separate experiments, the team found that mice carrying the fungal community in their gut displayed more social behavior than animals without these fungi.
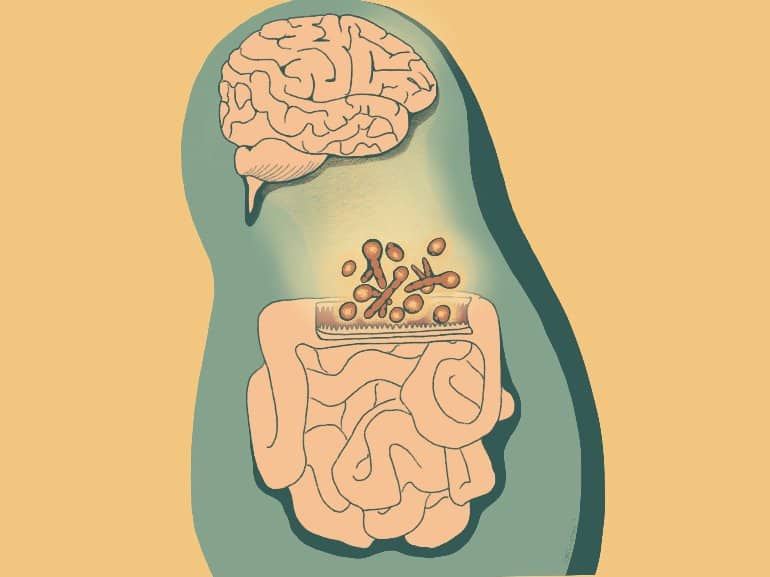
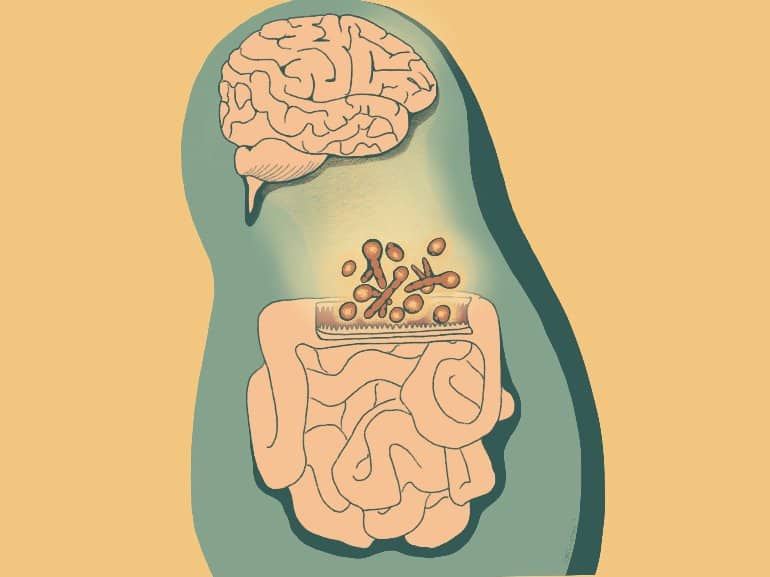
Both effects appear to stem from the animals’ own T cells, a type of immune cell. The fungi cause T cells to secrete two immune signaling proteins, cytokines IL-22 and IL-17. Fungi-induced IL-22 acts locally in the epithelium, strengthening its barrier function, while IL-17 enters the bloodstream and eventually reaches neurons, which have receptors for it. Mice lacking the IL-17 receptor in their neurons don’t exhibit the social effects of fungal colonization.
“There is this harmony—a kind of communication between or across different types of organisms,” Dr. Iliev said.
Now the investigators hope to explore that communication network further. “We are trying to go deeper into the mechanisms of this interaction, looking at the signals that are involved at the neuronal level in different brain regions,” said lead author Dr. Irina Leonardi, an instructor of immunology in medicine in Dr. Iliev’s laboratory at the Jill Roberts Institute for Research in IBD.
One tantalizing possibility is that different microbial communities in the gut could stimulate different regions of the brain and the immune system, exerting distinct effects on their hosts’ biology.
“This opens a whole new area to explore,” Dr. Iliev said.
About this microbiome and behavioral neuroscience research news
Author: Press Office
Source: Weill Cornell Medicine
Contact: Press Office – Weill Cornell Medicine
Image: The image is credited to Katarina Liberatore.
Original Research: Closed access.
“Mucosal fungi promote gut barrier function and social behavior via Type 17 immunity” by Iliyan Iliev et al. Cell
Abstract
Mucosal fungi promote gut barrier function and social behavior via Type 17 immunity
Highlights
- A specific community of fungi is present in the intestinal mucosa of humans and mice
- Mucosa-associated fungi (MAF) induce Type 17 immunity through T helper cells
- MAF protect mice against intestinal injury and infection via IL-22-dependent mechanisms
- MAF promote social behavior in mice through IL-17-mediated signaling in neurons
Summary
Fungal communities (the mycobiota) are an integral part of the gut microbiota, and the disruption of their integrity contributes to local and gut-distal pathologies. Yet, the mechanisms by which intestinal fungi promote homeostasis remain unclear.
We characterized the mycobiota biogeography along the gastrointestinal tract and identified a subset of fungi associated with the intestinal mucosa of mice and humans. Mucosa-associated fungi (MAF) reinforced intestinal epithelial function and protected mice against intestinal injury and bacterial infection.
Notably, intestinal colonization with a defined consortium of MAF promoted social behavior in mice. The gut-local effects on barrier function were dependent on IL-22 production by CD4+ T helper cells, whereas the effects on social behavior were mediated through IL-17R-dependent signaling in neurons.
Thus, the spatial organization of the gut mycobiota is associated with host-protective immunity and epithelial barrier function and might be a driver of the neuroimmune modulation of mouse behavior through complementary Type 17 immune mechanisms.
