
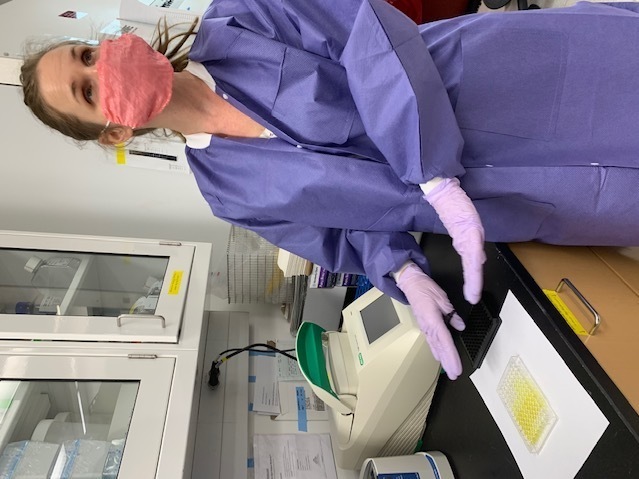
A research assistant with the Emerging Infectious Disease Branch (EIDB), at the Walter Reed Army Institute of Research (WRAIR), studies coronavirus protein samples, June 1, 2020. The EIDB is part of WRAIR’s effort to produce a COVID-19 vaccine candidate.
Mike Walters/U.S. Army
hide caption
toggle caption
Mike Walters/U.S. Army

A research assistant with the Emerging Infectious Disease Branch (EIDB), at the Walter Reed Army Institute of Research (WRAIR), studies coronavirus protein samples, June 1, 2020. The EIDB is part of WRAIR’s effort to produce a COVID-19 vaccine candidate.
Mike Walters/U.S. Army
Agi Hajduczki, a research scientist at the Walter Reed Army Institute of Infectious Diseases, opens a large freezer and takes out boxes of DNA. She is part of a team making a COVID-19 vaccine.
Hajduczki places a small, clear plastic tray under a piece of white paper on the table of her lab. The tray is dimpled. Pale yellow fluid can be seen under the dozens of dimples.
Some of the dimples are clearly more yellow than others.
“More yellow means more protein,” she explains. “So we’re basically trying to get mammalian cells to generate this protein for us, which would then eventually be used as the vaccine in a clinical trial so it kind of looks like the spike, the way it does in the real virus.”
The idea is that the immune system would get to know this protein — through the vaccine — and when the real virus hits, the immune system would know how to fight it.
Hajduczki became fascinated with viruses as a young girl in Hungary, watching her pathologist mother work on AIDS victims back in the early 1980s.
“So even, you know, when the world didn’t necessarily know about that this virus is happening like that was our dinner table conversation,” she says.
Now she has a young daughter, and has brought her to the lab during this pandemic, because like many parents around the country, Hajduczki and her husband are scrambling between work and childcare duties. Her voice breaks when she talks about the effect the virus is having on her work and family life.

Agi Hajduczki is a research scientist at the Walter Reed Army Institute of Infectious Diseases. She is part of a team working on a COVID-19 vaccine.
Tom Bowman/NPR
hide caption
toggle caption
Tom Bowman/NPR
Agi Hajduczki is a research scientist at the Walter Reed Army Institute of Infectious Diseases. She is part of a team working on a COVID-19 vaccine.
Tom Bowman/NPR
“It’s hard because like our whole lives have been upside down,” Hajduczki says. “We work in shifts, crazy hours, super amount of stress. But then, you know, when I go home, then dealing with the whole thing, like going to Trader Joe’s is like a two-hour excursion now, and I have a kid who has been at home from school…I have to kind of explain to her what’s going on.”
The vaccine Hajduczki’s working on will take some time, and won’t just target the current coronavirus. Human trials aren’t expected to start until later in the fall.
“The most cost effective and impactful public health tool”
A supply cart rolls down the long corridors at the institute just outside Washington, D.C, past labs and displays picturing nineteenth century scientists, letters and artifacts. There are closed doors with small signs on the wall. One says “Viral diseases.” Another simply, “Malaria.”
Inside one of these offices is the scientist heading Army efforts to aid in the race for a vaccine for the current pandemic: Kayvon Modjarrad, a civilian doctor. He’s a large man, with wireless glasses and an easygoing manner. His parents came from Iran to New York City back in the 1970s. He became interested in vaccines after taking a class as a medical student.
“I decided that I wanted to work on vaccines,” he says, “because it is the most cost effective and impactful public health tool that we have to saving lives.”
Modjarrad says he knew he was interested in medicine early on, “I got my first Fisher-Price doctor’s kit when I was four for the Persian New Year.”
Modjarrad is developing the Army’s coronavirus vaccines, but is also part of Operation Warp Speed, the government’s efforts to help private companies in the U.S. and internationally create coronavirus vaccines.
“So our institution and our network of sites here in the US and internationally are involved with many different companies,” he says.
That means sharing the Army’s expertise. Labs. Research animals. Locations for human trials, in Washington, D.C., San Diego and San Antonio. The Army also has partners and labs in Europe, Asia and Africa.
Modjarrad and other officials liken the vaccine effort to a horse race, with multiple companies coming out of the gate at the same time.
“Sort of whole of government approach has been putting our bets on multiple horses because we’re not interested in one particular horse,” he says. “We’re interested in a horse, at least one horse, making it across the finish line as fast as possible and being safe and effective and accessible for our entire public and population.”
Right now, several companies are working on the final phase three of human trials in developing a vaccine.
“It’s not like after the Phase three trial, ‘Hey, the vaccine is ready for everyone,'” Modjarrad says. “We start to phase it into the population and we still collect information on how people are responding to that vaccine until we get to a point where it becomes broadly available to the entire population.”

Kayvon Modjarrad is the scientist heading Army efforts to aid in the race for a vaccine for the current pandemic.
Samir Deshpande/Walter Reed Army Institute of Infectious Diseases
hide caption
toggle caption
Samir Deshpande/Walter Reed Army Institute of Infectious Diseases

Kayvon Modjarrad is the scientist heading Army efforts to aid in the race for a vaccine for the current pandemic.
Samir Deshpande/Walter Reed Army Institute of Infectious Diseases
Modjarrad says that what keeps him up at night “is that we go back to business as usual after this.” He says that this pandemic will pass, there will be multiple vaccines and people will be protected from this going on in the future, “but we have to be prepared” for future pandemics, he says, “these emerging infectious threats, Zika, Ebola coronavirus, a new strain of influenza. It’s not going away.”
The Army has a long history of producing vaccines. Modjarrad worked on vaccines for Zika and MERs. And one recently approved for Ebola.
And then there’s Walter Reed, the namesake. He was an Army major in the early 1900s who discovered that yellow fever was spread by mosquitos, not poor sanitation as some believed at the time. The virus had a devastating effect on soldiers and those working in tropical climates.
“So we sprayed and killed all mosquitoes,” Modjarrad says. “People weren’t dying. They built the Panama Canal.”
Diversity and inclusion
Modjarrad’s boss, Nelson Michael, director of the Center for Infectious Disease Research, is in a nearby office.
There are colored maps of Africa and the world in Michael’s office. A picture of him in his uniform, when he was an Army colonel. He’s often on the phone talking with participants of Operation Warp Speed, a name that has caused some to worry the speed has more to do with politics than science.
President Trump himself has fed that perception by suggesting a vaccine could be ready before Election Day, a view scientists say is unlikely.
“There’s been a lot of concern about what’s being sacrificed by moving so quickly,” he acknowledges. “And I can tell you, one thing is very clear it’s being sacrificed and it’s money.”
Michael says in the past vaccine development would take so long — often years — in part because companies and governments were wary of making an investment. A vaccine would be manufactured only after all approvals were done. The coronavirus changed all that.
“Now, everyone’s throwing financial caution to the winds and billions of dollars are in play,” Michael says. “But now you have, of course, a worldwide pandemic that’s costing trillions of dollars and impacting, you know, millions of people’s lives.”
Michael is also concerned about another controversy: Are human trials getting to a good cross section of the population, especially by race?
“If you look at the impact of the SARS-CoV-2 infection and the disease it causes, COVID-19, there is a disproportional impact on people of color in the United States,” he says. “So you are at much greater risk if you’re over 65, if you have comorbidities, hypertension, obesity.”
Many of the comorbidities that are particularly present in minority segments of society.
“Blacks and Latin and Native populations in our country are at substantially higher risk,” he says. “So it’s more important than ever that we have diversity and inclusion in these studies.”
All those working on the vaccine, whether private or government efforts “want to do better. I can tell you that.”

Nelson Michael, director of the Center for Infectious Disease Research, says a strong public health campaign will be needed to convince Americans the vaccine is safe and effective.
Tom Bowman/NPR
hide caption
toggle caption
Tom Bowman/NPR

Nelson Michael, director of the Center for Infectious Disease Research, says a strong public health campaign will be needed to convince Americans the vaccine is safe and effective.
Tom Bowman/NPR
Michael acknowledges the suspicions especially in the Black community, who have been victims of government studies. The most horrific was the Tuskegee Experiment, which from the 1930s in the 1970s followed hundreds of Black men with syphilis over the course of their lives, failing to tell them about the diagnosis and refusing to treat them.
For this vaccine, says Michael, the government has created community engagement groups to reach out to African American and Native Americans in particular.
“I’d say Native populations are also very mistrustful because of the history,” Michael adds. “And you know there are lots of issues, of course, that are hitting our country right now all at the same time, systemic racism.”
But he says there likely to be an even greater challenge once a vaccine is approved.
“I am more concerned about how we’re going to execute a vaccine campaign than I am about how we’re going to test this vaccine,” he says. “How are we going to convince Americans that they should sign up for their vaccine?”
Some polls show at least 30% of Americans say they won’t take the vaccine. There are scientists who say at least 40% of Americans must take the vaccine. Michael puts that percentage even higher.
“What we really need is to have somewhere between 70% and 90% of Americans that either have been vaccinated and have immunity that way or have been exposed and survived and have immunity because of natural infection,” he says.
A vaccine from at least one of the private companies is expected earlier next year. The Army also continues to work on its own vaccine that can target future coronaviruses.
No matter what, a strong public health campaign will be needed, Michael says, to convince Americans the vaccine is safe and effective. One part of that is to reach out to those people Americans tend to trust most: Their family doctor.

