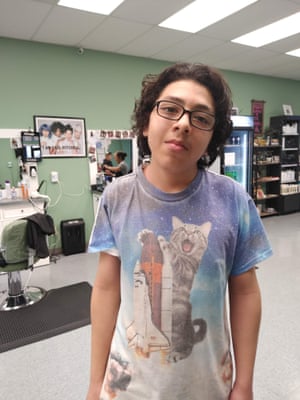
Well before the pandemic upended his world, Antonio Luna struck his new therapist Paul Jamison as a challenge.
At his intake appointment in late October 2019, Luna, a skinny, shy 16-year-old with dark, wavy hair and an oversized leather jacket, talked about his struggles with suicidal urges and the plans he had made to act on his distress. After one close call in May, he had been hospitalized for more than a week. He was still feeling hopeless and beset by self-destructive thoughts. When Jamison asked about his goals for therapy, Luna replied, “Try to find a reason to live.”
Luna, who had been diagnosed with autism spectrum disorder as a child, came across as guarded but willing to work with Jamison in creating a plan to stay safe. “I’ll tend to lie that I’m fine but really I’m not,” Luna conceded to Jamison in their first session. He answered the therapist’s questions about his prior experiences in the mental health system and shared information about his tough childhood. While he did not completely trust his new therapist, he at least felt secure at the clinic. It was what he knew.
The one-story, beige and white brick building just south of downtown Nashville, Tennessee was a familiar and soothing place. It was run by Centerstone, a nonprofit that operates more than 170 mental health clinics across the South and Midwest. Luna had gone there for years starting at age 10 to calm his in-the-red emotions and to decode the complicated social cues at school. His family had since moved about an hour north to Springfield, which was closer to other Centerstone locations. But Luna insisted on returning to this particular clinic.
His mother, Elizabeth Lucatero, 42, and stepfather, Kevin Poole, 48, drove him to each session. There were always jokes about who was the better driver, Mom or Dad (the answer was always Dad). From the backseat, Luna kept the conversation light and unremarkable. His parents believed these commutes showed their son the importance of seeking help for one’s problems. Lucatero had a long history with mental illness and she didn’t want her son to suffer as she had.

After therapy, Luna knew to expect a reward, an ice-cream from Sonic or a steak and rice dinner from a favorite Mexican place, interludes that granted time to decompress before the long drive home. His parents tried to keep the conversation upbeat. “I always told him to keep his head up, to keep going, that things were going to get better,” Lucatero said.
Luna’s treatment was covered by Lucatero, who was on the state’s public assistance health insurance. They were lucky. Even before the pandemic fueled an unmeetable surge in demand for youth mental health services, there have never been enough therapists to treat children and teens. Parents agonize over waiting lists, calls to clinics that go unreturned, and the promise that the next referral will pan out. And even when there are openings, families contend with a dearth of providers who accept insurance and are willing to treat a young person with a complex psychiatric history.
Not only does the nonprofit take teens and adults at risk for suicide, it strives to keep them engaged in therapy. If suicidal clients miss a session, they get a check-in call from Centerstone to schedule a new appointment. The manager of Luna’s clinic, Susan Seabourn, secured grant funding to pay for indigent clients’ bus tokens and copays in the hopes of boosting attendance. Luna was a beneficiary of the careful attention the clinic aspired to give.
At that first instake session, Luna was deemed a suicide risk and the clinic mobilized a team to watch over his case. The high-risk status entitled him to regular therapy and medication management appointments. A Centerstone staffer spoke with Lucatero about removing guns and other hazards from their home, and she said their firearms were locked away at a friend’s house. Over the course of a few months, Luna began to talk about his moments of intense suicidal thoughts and what overwhelmed him. He compared his depression to having a migraine. “There’s just so much going on in my mind,” he explained to Jamison. “It literally hurts my head.”
During a session in mid-February 2020, he admitted to Jamison that he had thought about suicide the previous night and had devised a plan to hang himself from a tree in the woods near his house. Jamison called in Seabourn, who was skilled at working with kids, to counsel the teen. Luna agreed to avoid the woods and consented to let Seabourn coordinate with his brother to keep an eye out. Luna eventually reported that his suicidal thoughts had waned. Therapy seemed to be working.
But in March 2020, the pandemic shuttered normal life. Luna’s high school closed for spring break and never reopened. His church closed, as did the public library where he had been a regular in the young adult section. And overnight, with no playbook or precedent, Centerstone went remote, replacing the vast majority of face-to-face services with Zoom rooms and phone calls.
For Luna, this meant no more weekly trips to one of the few places he could be himself unconditionally, no more steak and rice dinners and special family time. The structure he depended on vanished.
Despite his ambivalence, Luna was willing to try a new routine. In March, he began teletherapy.
•••
Like the vast majority of mental health systems across the US, Centerstone embarked on an unparalleled experiment: the clinic had to repurpose its traditional offerings using smart phones and video links. These tools had to suffice to treat and manage its high-risk clients – the victims of trauma and domestic abuse, the chronically suicidal, and those who were losing loved ones to the pandemic. The stakes were especially high for children and teenagers, as hospitals around the country experienced dramatic increases in pediatric psychiatric emergencies.
Becky Stoll, vice-president for crisis and disaster management for Centerstone, tried to view the lockdown as an opportunity. For years she had wanted to offer teletherapy services as a way to expand Centerstone’s reach. “Covid-19 has pushed us into the largest beta test that we ever could have hoped for,” she told me in the spring of 2020. With each passing week, Centerstone’s staff worked long hours to stabilize and expand its pandemic response.
Unreachable places suddenly became reachable. People in pain could simply log on or pick up the phone for a session. For many, teletherapy proved to be as effective as in-person treatment, and it had the power to ease barriers like transportation costs and commute times. After therapy went virtual, the nonprofit experienced a steady increase in people showing up for new intakes – up by as much as 20% a month. The new protocols, however, took a toll on staff. Every day, therapists were conducting sessions in their bedrooms, basements, and living rooms, often without a break between the next Zoom hit.
Heather Kamper, a licensed clinical social worker who recently left Centerstone, described the experience as “robotic”. Absent the structure, and etiquette, of in-person therapy, some sessions felt ineffectual, Centerstone therapists said, even like a waste of their client’s time. Clients struggled to find private places to speak. They called from the road, and from the aisles of the grocery store, and from living rooms crowded with family. Some Zoomed without clothes. One victim of domestic abuse had to arrange to do therapy from inside a closet in her home.
Going remote made Kamper appreciate how much she relied on physical cues to gauge her clients’ well-being. She was accustomed to calmly sitting with her suicidal patients while reassuring them that their crises were temporary and could be overcome. She’d find a way to bring them down from this painful state. Now, no matter how hard she concentrated, when there were breakthroughs, she couldn’t feel them. When one of her long-term clients, a woman in her 50s, admitted that her suicidal thoughts were back, Kamper’s own anxiety spiked. In that moment, both patient and provider felt unmoored.
“I miss our Saturdays,” the client told Kamper. “I want to be in a room with you. What if I die? What if you die?”
•••
Luna struggled with the transition to teletherapy. He was no longer just a client but an unwitting participant in this unfolding virtual experiment. When he first began therapy at Centerstone about seven years prior at age 10, in-person interactions played a large role in his treatment and in his ability to establish trust in his therapists. Luna’s sessions involved more than just talking, they also included physical observations as well as games like Connect Four and Battleship. He was able to open up about his deepest traumas and anxieties as he tried to make sense of an unjust world.
At his first session in late 2013, he wept while describing how his estranged biological father used to mistreat him (Lucatero said he could be abusive and violent). Later, he shared that he was worried about his mother because she wasn’t eating and that he was being bullied at school. During this time, he also told a therapist he had suicidal thoughts.
Progress was marked by how often he pulled his hair as a coping mechanism or whether he was able to tame his outbursts in school. “Our lives never got easier but it was easier because we knew exactly what was going on,” Lucatero said. By the end of seventh grade, Luna’s therapist noted: “Client has done well in school this year with no incidents of mobile crisis or police being called. No elopement from school or hiding under furniture or cars in the parking lot.”
Luna insisted on conducting his teletherapy sessions by phone, rather than video, and initially maintained that he felt safe. Of his suicidal thoughts, he remarked: “I don’t feel like I have to work on that stuff anymore.” But a few weeks later in early April, his mood soured. The lockdowns and all that he was missing were on his mind. He told Jamison he felt angry that “something has been taken away from me.” The two brainstormed strategies for when his anger flared up like listening to music, taking a shower, or cycling. But that session, Jamison thought, could have gone deeper. In his notes, Jamison wondered if conducting the session by phone “could have hindered rapport and communication.” The session lasted only 30 minutes.
On their next call two weeks later, Luna seemed especially concerned about his mental health. He reported that he was starting to have auditory hallucinations, like someone was making him feel as if he wanted to die. “I’m satisfied with life,” Luna said. “It’s like someone else is thinking for me.” Jamison suggested meditation to ward off the voice in his head.
Susan Seabourn, the clinic manager, and Jamison recognized that Luna needed extra support. They repeatedly invited him to join their virtual teen therapy group – he did not have to talk or turn on the camera, they said. But it was to no avail. They had good reason to be concerned. Centerstone was seeing an increase in suicides among its 21 and under clients, up from three in 2019 to five between May and December of 2020.
This ratcheting up of acute distress roughly tracks what was taking place across the country. While there is still much to learn about all the ways the pandemic has affected children and taxed an already inadequate mental health system, between isolation, anxiety, and mounting household-level stress, young people like Luna have experienced and continue to experience worsening mental health outcomes.
In a national survey of parents, 46% said they noticed a decline in their teenager’s mental health. Roughly a third of teen girls and a fifth of teen boys had increased symptoms of depression, poor sleep, and withdrawing from family. The pandemic further coincided with a time of national upheaval and instability. Systemic issues like racial injustice and financial precarity can increase stress at home, all at a time when kids have nowhere to go, explained Jeffrey Bridge, Director of the Center for Suicide Prevention and Research at Nationwide Children’s Hospital.
Across the US, hospital emergency departments reported seeing more suicidal kids than they had in the year prior to the pandemic. The situation got so dire that the CEO of one Colorado children’s hospital declared a state of emergency. Children’s Hospital at Montefiore, the largest children’s hospital in the Bronx, saw an 80 percent increase in suicide attempts during the lockdown months over the previous year for patients under 21 years old, according to Dr Lisa Hutchison, an attending psychiatrist at Montefiore Medical Center.
“I think everyone can agree that telehealth is not the same, especially for children living in poverty where access to screens and Wi-Fi and privacy are limited,” Hutchison said. “These challenges are not a reflection of telehealth’s failures, but rather reflect ongoing socioeconomic issues that continue to create barriers to care.”
For children with more serious behavioral issues and psychiatric histories, virtual care might not be best for them or even possible. “They’re hyperactive, they’re dysregulated, they really struggle to try and connect with people on screen,” said Meredith Gansner, a child and adolescent psychiatrist at Cambridge Health Alliance in Massachusetts. For children who’ve experienced trauma, she added, it can be hard for them to even look at themselves on screen.
Luna spent most of the lockdown at the home of his partner, Alex Fulton, a fellow 16-year-old who uses the pronoun they. Their days were spent in Fulton’s bedroom playing out endless Dungeons & Dragons scenarios or building worlds in Minecraft. The two shared a similar mental health history that included hospitalization and years of being burdened by chronic suicidal thoughts. Fulton was his sympathetic ear, the one person who could potentially understand what he was going through.
During Luna’s therapy calls with Jamison, Fulton was often present. The sessions were sometimes helpful, Fulton recalled, though not in the way Jamison may have intended. Luna hated to talk about what was bothering him, Fulton explained, so much so that he’d try and talk about anything else, and his mind would shift out of his self-hatred. The distraction could sometimes leave him in a better mood.
But not always. In early May, Luna told Jamison his suicidal thoughts had become overwhelming. He asked Luna if he wanted to talk to the mobile crisis team or the police. Luna told his therapist to call the police. Their phone connection then dropped.
Luna was at Fulton’s house at the time. His stepfather, Kevin Poole, had just arrived and was idling outside waiting to pick Luna up when Jamison called him. Poole assured Jamison that he would take his son to the hospital. But Jamison called 911 anyway and requested the police do a “welfare check.” Therapists will call the police to possibly interrupt a suicide attempt or check on a client they think might be in danger of making an attempt. The police can do an assessment on the spot and decide whether the client needs to be transported to the hospital. But by calling the police, the therapist risks alienating the client who can feel humiliated and exposed by the experience.
The police arrived and ordered Luna to come with them. To Fulton, the cops seemed indifferent and maybe a little annoyed—like they would rather be anywhere else. Luna hardly looked at them, he just followed their commands. This was the one time since the lockdown that Centerstone had intervened into his physical world.
When the officers got outside with Luna, they told Poole to take him to the hospital. Luna seemed upset and shaken by the experience, “like he wanted to kill the world,” Poole said. On the ride to the hospital, Luna became defiant. There was no way the hospital was going to commit him. “I won’t talk to them,” Poole recalls Luna saying. “I won’t tell them anything. They can’t keep me.”
At the hospital, Poole pulled the nurses aside and told them of Luna’s intent. But it didn’t make a difference. If Luna did not want to talk to them, they told Poole, there was nothing they could do. Luna was soon released.
•••
Even under normal circumstances, clinicians have difficulty reaching those who become paranoid and mistrustful. During the pandemic, clinicians had to work especially hard just to get these clients to answer their calls and to stay on the line. Some hung up on them and weren’t reachable again.
In these cases, clinicians need uninterrupted time in the same room as their clients. In person, therapists can gauge eye contact, body language, and even hygiene to determine whether there’s an immediate concern or something more benign, Gansner said. Kids, she noted, have an especially hard time distinguishing between what might be a really loud inner voice and what might be a hallucination. This can be terrifying for anyone, let alone a 17-year-old.
Jamison, who no longer works at Centerstone, said he had a caseload of 150 clients, and of those he was regularly seeing 80. There was hardly time to think about clients ahead of their teletherapy sessions. The pressure fell hardest on clinicians, the majority of whom are paid fee-for-service, which means their wages are tied to productivity. Limiting therapy with Luna to phone calls made it even more challenging because Luna spoke in a monotone.
The small circle of family and friends around Luna noticed a change in him after the police welfare check. At dinner, he pushed food around his plate, merely pretending to eat. He withdrew from conversations more and more. Lucatero thought she was watching her son become a ghost. “I just didn’t know how to fix him,” she said.
Luna was still looking for answers from Centerstone. Five days after the incident, with Jamison’s prompting, the two explored Luna’s underlying depression and Luna thought maybe his anxieties were linked to his traumatic childhood. He added that he felt really down and was hopeless about his future. Jamison marked him, again, as a suicide risk.
After one abbreviated session, Jamison’s notes contained a familiar refrain: “client seemed tired today and was not fully engaged in session.” Luna would open up just for a moment, the way a flat stone skips over the water before plunging back into the deep. The two were stuck. The onus was on the therapist to get them unstuck.
“I don’t know if doing sessions on telehealth really made that much of a difference in his care,” Jamison said. “Overall I think we can connect with clients better when we can see them, when we are in the same room with them.”
As spring inched closer to summer, Luna’s belief in therapy may have begun to falter. He didn’t answer his phone for two consecutive sessions. In a meeting with his medication provider at Centerstone, he complained of having an “anxiety attack.” He said his heart rate had spiked and he had trouble breathing. He had felt like he was dying. He seemed lost, describing his mood as “pretty bad” and said he hadn’t gotten much sleep. The provider recorded him as “markedly ill.”
When he next spoke to Jamison, he told his therapist: “I’m super paranoid, and I’ve gotten to the point where I can’t trust anybody.” His mood persisted into their next session, where he said he had a “mental breakdown” the day before and still had suicidal thoughts periodically. Luna wouldn’t elaborate further. Again, the therapist wrote that Luna “presented with a flat mood, gave minimal responses.”
Their next therapy call was scheduled for a month later. From what Jamison could remember, he just didn’t have another session time available. He only had time enough, he said, to call him once to check on him. But when he did call, Luna didn’t pick up.
Meanwhile, Luna’s mood swings were only getting more extreme. When Lucatero and Poole took Luna and Fulton to Barnes & Noble, it was the happiest they had seen him in a while. But the next day, on July 3, Luna was so agitated that Lucatero left work to check on him. At home, she noticed that he seemed different, more desperate and more hopeless than usual. He paced their house, unable to calm down. But he had a solution. He asked his parents if they could drive him to the hospital.
“He was reaching out for help,” Lucatero thought, like she had taught him. Poole had a shift at UPS that he couldn’t afford to miss, but Lucatero told Luna she would quickly clock out of her shift at a nearby convenience store then come home and take him to the hospital. She’d be back in just a few minutes, 10 minutes at most. She told him she loved him. “I’ll be right back,” she said. He said he was going to get dressed so he’d be ready to go to the hospital. His two siblings were home too.
Luna rummaged through his parents’ bedroom until he found his stepfather’s gun. It was the one gun they kept because Poole worked the late shift and Lucatero felt like they needed protection in the home; they thought it was secure in a lockbox under their bed. On her way home, Lucatero noticed her phone was buzzing with texts and calls. She hit the gas and ignored them. When she arrived home, she found her daughter desperately trying to rouse Luna’s body.
Paramedics rushed Luna to the hospital. But there was nothing the doctors could do. Lucatero asked for a chaplain who then escorted her to her son’s bedside. After they prayed over his body, she asked to be left alone with her “Tony.” She held his hand and tried to brush back his hair. She told him it was OK for him to go. After his death was confirmed, a nurse handed her a printout of her son’s last steady heartbeats and told her it would make a great tattoo which she later had inked on her body.
Within days of her son’s death, Lucatero made the 10-minute drive back to the convenience store to take a shift. She had to endure customers who told her that her son was going to hell or expressed relief that he didn’t kill anyone else before taking his own life. There were times when she had to hide in a back room to take refuge from their judgement.
Luna was a victim of Covid. He may not have been one of the more than 700,000 Americans who have died from the virus, but the virus created the circumstances that led to his death – putting physical and psychological distance between him and the help he needed, upending the routines he had come to rely on for security and comfort.
With the spread of increasingly contagious variants and too many Americans still refusing vaccination, the pandemic will define our lives for the foreseeable future. It will continue to create unbearable environments for teenagers. It is impossible to know if the continuation of his in-person therapy would have prevented Luna’s suicide, but it’s devastating to have to wonder.
Fulton worried that people would view Luna’s death as a personal failing and not what it really was. “I feel like it was just a failure of the whole world,” Fulton said, “and every single thing that we had turned against us.”