The delta variant is driving up coronavirus cases in California, landing the Bay Area on a federal “hot spot” watch list and spurring renewed urgency to get shots into the arms of people who haven’t been vaccinated, even in areas where immunization rates are already high.
In San Francisco, public health officials are now requiring all workers at hospitals, nursing homes, jails and shelters to be vaccinated by Sept. 15. That’s a shift from an earlier order that mandated vaccination only after at least one vaccine was fully approved by the Food and Drug Administration, which now allows the shots under emergency authorization. Stanford Medicine announced a similar policy shift Friday.
The moves come as cases have more than doubled in parts of the state, including Alameda and Los Angeles counties, and several large outbreaks have been linked to the highly infectious delta variant. Sonoma County on Friday reported worrying signs of a surge in cases and hospitalizations, plus five COVID-19 deaths last week, the most since February. A Santa Rosa homeless shelter was closed after reporting a few positive cases July 2 — since then, about a third of its 150 residents have tested positive, most with confirmed delta cases. Few of the residents were vaccinated.
“There’s no health order that’s going to prevent every infection,” Dr. Susan Philip, the San Francisco health officer, said after issuing the new vaccination requirement for some workers. But with delta-fueled cases climbing, “the vaccines are a firewall against COVID-19 in our most vulnerable populations,” she said.
The updated vaccine mandate applies to people who work in any high-risk setting in San Francisco, including those not run by the city. That includes, for example, private hospitals and nursing homes. It does not apply to all city workers — including police and firefighters — who will be required to get vaccinated only after vaccines are approved by the FDA.
Although San Francisco already has among the highest vaccination rates in California, Philip said virtually everyone must be inoculated in congregate settings or in places that house many high-risk people. At Laguna Honda, the city’s largest skilled nursing home with about 720 residents, 86% of staffers are fully vaccinated.
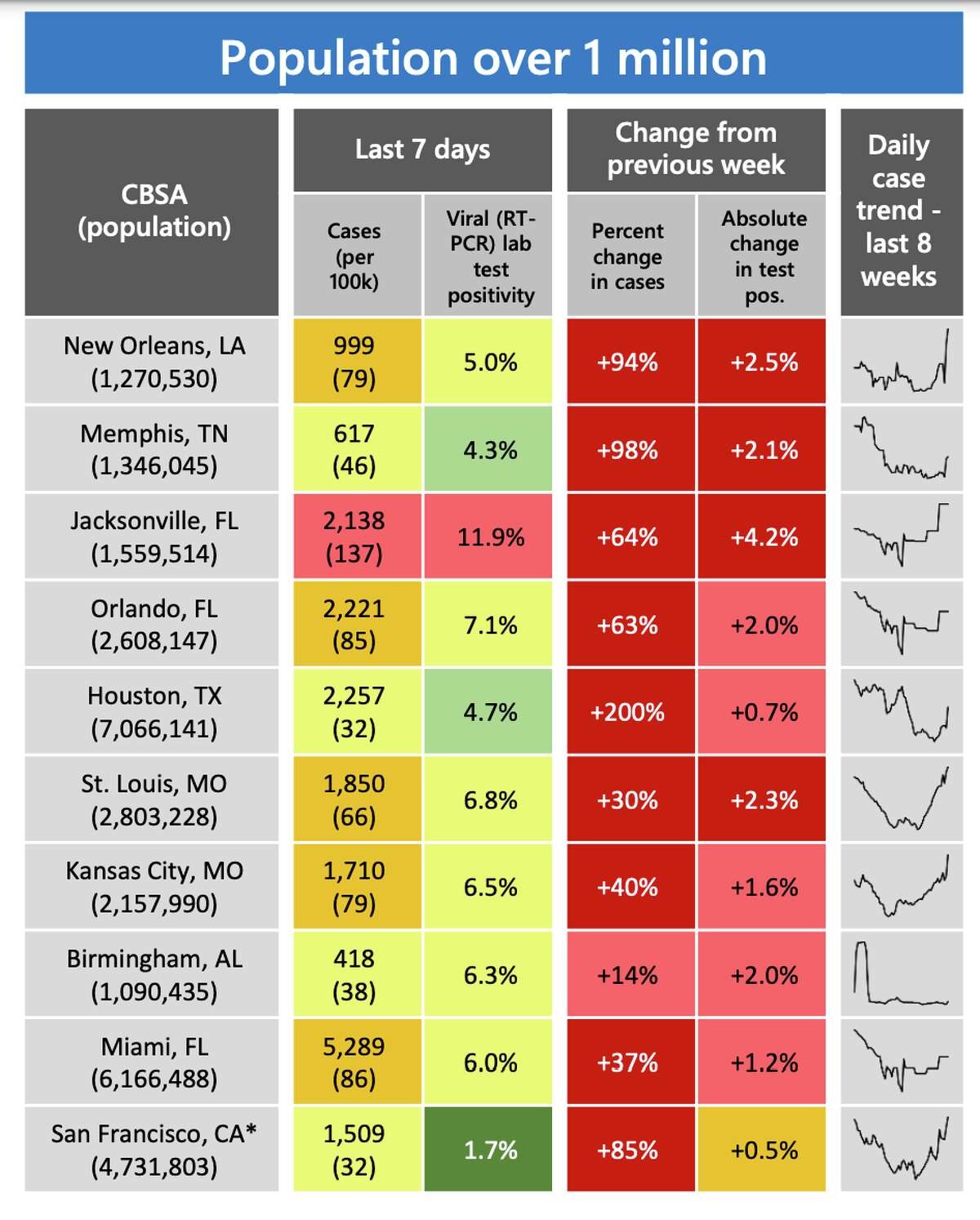
This chart from the CDC’s Community Profile Report shows the San Francisco Bay Area as one of the areas with the largest recent increase in disease burden for its population size.
CDCAt Stanford, all hospital and other health system employees will be required to be vaccinated effective Aug. 15, said spokesperson Lisa Kim. “We join an increasing number of health systems nationally in taking this action with urgency, particularly in light of the emerging threat of highly infectious variants,” she said.
Nationwide, cases are spiking in regions that are under-vaccinated as the delta variant dominates, and federal health officials are concerned that uncontrolled spread of the virus could spawn more mutations. The delta variant is thought to be up to twice as infectious as the original strain of the coronavirus, and 40% to 60% more infectious than the alpha variant, which dominated in the U.S. through the spring.
Delta makes up roughly 40% of new cases in California, but the state should be less vulnerable to surges in cases due to its overall high vaccination rates, combined with high levels of natural immunity from people who have already been infected.
Cases have climbed statewide since June 15, when California lifted almost all public health restrictions — from an average of about 2.5 cases per 100,000 residents a day to 4 per 100,000 recently. Bay Area counties are seeing similar increases.
Those are still relatively low rates, but on Friday, the federal Centers for Disease Control and Prevention listed the Bay Area as an “emerging hot spot” due to rising case numbers over the past week. According to the CDC, cases have climbed 85% for the region week over week.
The positive test rate is still low, at 1.7%, especially compared with other hot spots, which range from 4.3% in Memphis, Tenn., to 11.9% in Jacksonville, Fla.
But there are troubling signs in some Bay Area counties, including Sonoma, where the positive test rate is 3.1%, health officials said. Of the five deaths reported last week, four were people who hadn’t been vaccinated. The fifth was a man who was fully vaccinated, but he was over age 90 and had other underlying health problems, which underscores the importance of continuing to protect the most vulnerable residents, health officials said.
“The numbers are trending in the wrong direction,” said Dr. Sundari Mase, the Sonoma County health officer. “Nearly all of our recent COVID cases, hospitalizations and deaths have involved unvaccinated individuals. Getting vaccinated is the most important thing you can do to protect yourself and the community.”
Hospitalizations have increased in the state and locally — by almost 50% in the Bay Area and about 37% across California since June 15. But they’re still down more than 90% from the winter peaks. Hospitalization numbers are similar to those seen during other lulls in the pandemic — the difference this time is that there are almost no health restrictions like mask mandates and bans on public gatherings.
That’s a sign the vaccines are holding up, infectious disease experts said. The optimism is reinforced by the latest death tolls, which have remained at or close to their lowest levels since the pandemic began. Statewide and nationally, more than 99% of people who have died of COVID in recent months were not fully vaccinated.
“The vaccines are performing extremely well, even as the virus throws its best punches at us,” said Dr. Warner Greene, a senior investigator with the Gladstone Institutes in San Francisco.
Despite evidence in international studies that the vaccines are somewhat weakened against the delta variant, they are maintaining strong protection against the most serious outcomes of infection, experts said.
The most discouraging study to come out so far — a report from Israel this week — suggested that the Pfizer vaccine was only about 64% effective at preventing infection, but was still more than 90% effective at preventing serious illness. Other vaccines, including those made by Moderna and Johnson & Johnson, need more study but also appear to be holding up well in preventing hospitalizations and deaths.
“The goal of the vaccines is to prevent severe disease, hospitalization and death. And we have access to three fantastic vaccines that are safe and effective,” said Dr. Upinder Singh, division chief of infectious diseases at Stanford Health.
Singh said she recently treated a 25-year-old man who was fully vaccinated and had tested positive. He was “quite symptomatic,” Singh said, but “this person won’t die. He has a bad cold.”
That’s a critical distinction as places with high vaccination rates maneuver through reopenings and figure out how to co-exist with the coronavirus. Singh said the patient she treated had been going to clubs and other places unmasked, which is reasonable for a young healthy person who is fully vaccinated, especially given the relatively low case rates in the Bay Area, she noted.
But it’s not entirely without risk. Increasingly, people are having to make those assessments for themselves.
“I’m fully vaccinated and I don’t feel comfortable going to the grocery store or even outdoors at the farmers market where it’s really crowded, so I wear a mask in those situations,” said Dr. Dean Blumberg, chief of pediatric infectious diseases at UC Davis Health. “But a lot of people aren’t wearing masks, and that’s fine for them. We have to let people know what the risks are and recognize that everyone has different risk tolerance and different circumstances.”
Oakland resident Tania Yarema had a solid grasp of the risks, but she was still dismayed when she and her 7-year-old son, Julian, became infected at the end of June. Yarema is a nurse practitioner who works in intensive care, and she’s been fully vaccinated since December.
She was still being careful, she said, since Julian couldn’t yet be vaccinated. But with case rates so low across the region, the boy had been to a few indoor gatherings, including visits with family and a trip to the Legoland Discovery Center in Milpitas — always with a mask on, Yarema said.
She doesn’t know where he was exposed to the virus, but he woke up with a high fever on June 29. Yarema developed symptoms a few days later. Julian was hospitalized for five days, which was “brutal,” Yarema said, but by Thursday he seemed back to normal.
“I’m awesome,” he called out while his mom was interviewed by phone.
“I’m still pretty short of breath. And other than that, just super tired and feeling crappy,” Yarema said.
Although she’s frustrated she was infected at all, she believes the vaccine probably kept her symptoms milder than they might have been.
“I can’t imagine what this would be like without that vaccination,” Yarema said. “I probably wouldn’t have done well.”
San Francisco Chronicle staff writer Catherine Ho contributed to this report.
Erin Allday is a San Francisco Chronicle staff writer. Email: eallday@sfchronicle.com Twitter: @erinallday


